ANTIGENS
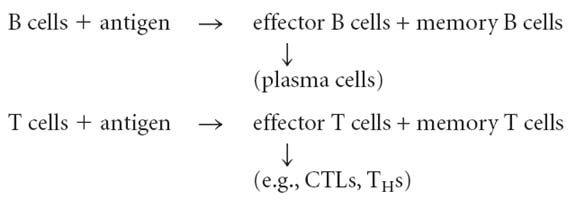
They are named so because they have an ability to induce antibody generation. There are two terms interchangeably used. They are antigens and immunogens. Antigens are foreign substances which an ability only to bind with products of immune response i.e. antibodies and T cells. Immunogens are foreign substances which have an ability to induce production of immune response products like antibodies and activated T cells and to bind with them. Because of this, “all immunogens are antigens but not all antigens are immunogens”. But in an immunology book, usually antigen term is used to explain both antigen and immunogen.
TYPES OF ANTIGENS:
1. Sequestered antigens:
These antigens are secluded or sequestered in capsule i.e. it is not exposed to immune system during development or produced. So, when they exposed, they elicit immune response. Ex: Lens proteins and sperm proteins.
2. Neoantigens:
Neoantigens are newly produced antigens i.e. normal agents become antigens. They are formed due to the change in the chemical, physical and biological status of the agents. Ex: Penicillin can be converted to neoantigen when it bound with protein. It is otherwise known as altered antigen.
3. Hereophile or Heterogenic or Cross reactive antigen:
These antigens interact with antibodies produced against another antigen. For ex: Forssman antigen. These antigens are present on mucosal cells of GI tract and RBCs of horse. When an antibody produced against any one of the antigens, antibodies will interact with the other antigens also. Thus these antigens are known as cross reactive antigens. The phenomenon is known as cross reaction. The function of binding of antibody to an antigen to which it is not produced known as cross reactivity.
4. Mitogens:
Since some mitogens activate immune cells, they can be considered as antigens. Mitogen causes cancer due to inducing cell division. EX: Lipopolysaccharides induce B cell proliferation, Concanavalin – A (CON A) and Phytohemagglutinin (PHA) induces T cell proliferation and Pokeweed mitogen (PWM) induces both T and B cell proliferation.
5. Superantigens:
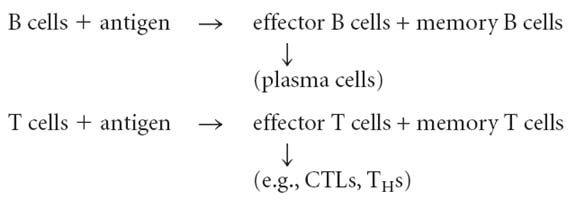
These antigens activate T cells non-specifically. They are of two types namely exogenous and endogenous superantigens.
a. Exogenous superantigens:
They are capable of activating T cell – APC complex exogenously i.e. they bound to surface of APC cells and activate T cells when they interact with APC cells. These antigens are not processed. Ex: TSST-1 (Toxic shock syndrome toxin – 1) produced from staphylococcus.
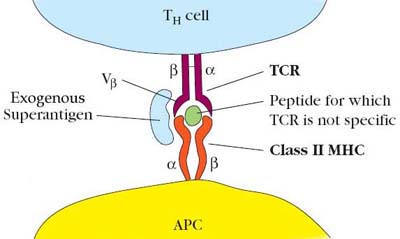
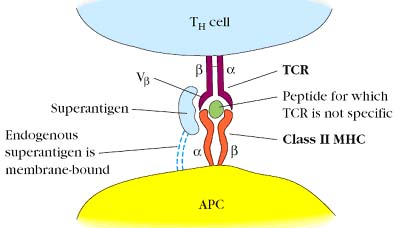
b. Endogenous superantigens:
They are called endogenous because they are processed and presented by APC cells in an irregular manner i.e. superantigens are not presented through MHC molecules but they are present outside the MHC molecules. But they activate TH cells but interacting a chain of MHC and Vb region of b chain of TCR of T cells. For example: Mouse mammary tumor viral (MMTV) antigens. One group, encoded by mouse mammary tumor virus (MTV), can integrate into the DNA of certain inbred mouse strains; after integration, retroviral proteins are expressed on the membrane of the infected cells. These viral proteins, called minor lymphocyte stimulating (Mls) determinants, bind particular Vb sequences in T-cell receptors and crosslink the TCR to a class II MHC molecule. Four Mls superantigens, originating in different MTV strains, have been identified.
Since superantigens activate T cells nonspecifically, the function is referred as co-reactivity.
6. Exogenous antigens:
These antigens are usually secretary products of microbes or soluble antigens. It is usually present outside the host cell and it is processed by APC cells and presented through MHC – II molecules. For example: exotoxins (diphtheria toxin from Cornebacterium diptheriae).
7. Endogenous antigens:
They are usually microbes which are present inside the cell or particulate antigen. These antigens are processed and presented by MHC – I molecules. For example: Virus and endotoxins.
8. T cell dependent antigens:
These antigens require T cells especially TH cells to induce immune response. For example: soluble proteins.
9. T cell independent antigens:
T cell independent antigens require T cells partially or not to induce immune response. On this basis, they are classified into two types, T cell independent antigen – I and T cell independent antigen – II.
a. T cell independent antigen – I:
It does not require T cell to induce immune response. For example: Lipopolysaccharides.
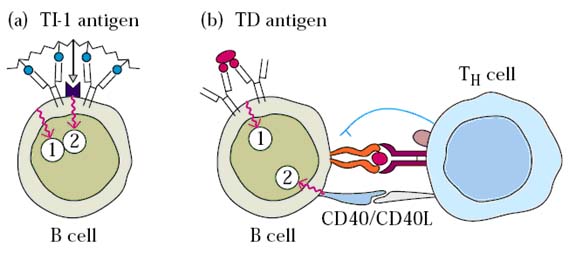
b. T cell independent antigen – II:
It does not require direct contact of T cells but cytokines produced by them to induce immune response. For example: Cell wall polysaccharides and glycoproteins.
10. Allergens:
Antigens are responsible for allergic response is called allergens. For example: Pollens.
11. Autogens:
Those antigens which are capable of inducing auto immune disorders are known as autogens.
12. Self antigens:
They are not originally antigens. They are normal cell surface components and proteins of normal host. But they can be converted to antigens like autogens.
13. Haptens:
Haptens are otherwise known as incomplete antigens or partial antigens because they are unable to elicit immune response by itself, but they can gain this ability when bind with carrier molecule. Karl Landsteiner determined Haptens through his studies. For example: Dinitrophenol (DNP). When it is injected as such it is unable to induce antibody production against itself but when DNP- Bovine serum albumin (BSA) complex injected it can able to induce antibody production against BSA, DNP and DNP-BSA complex.
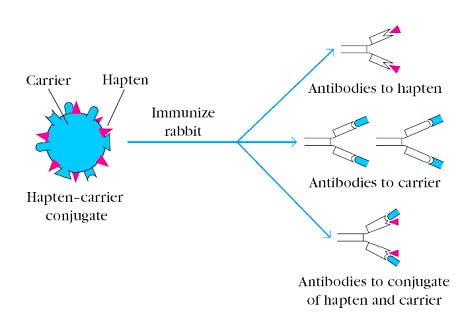
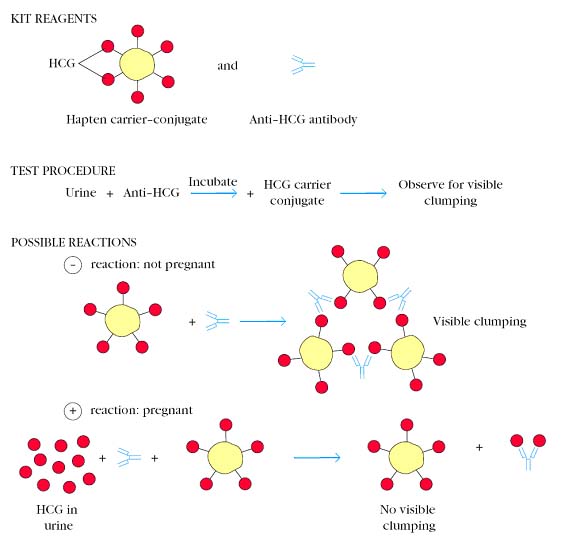
Haptens are behaved differently in different hosts. For example: Pneumococcal polysaccharide, when it is attached with carrier and injected it will elicit immune response in cow and human but not in rabbit. Hapten-carrier phenomenon utilized in some diagnostic test e.g. Maternity test, Human chorionic Gonadotropin treated as Hapten. This is used to confirm pregnancy. After few weeks of fertilization HCG appears in urine. This factor is utilized in the test. Antibodies against HCG allowed reacting with HCG in urine if present. After suitable time interval, RBC coated with HCG added to the above mixture. Appearance of agglutination is tested. If agglutination present, pregnancy is not confirmed and vice versa.
ANTIGENICITY AND IMMUNOGENICITY:
Ability of an antigen to induce immune response is known as antigenicity. Ability of immunogens to induce immune response is known as immunogenicity. These two terms used interchangeably.
Factors affecting Immunogenicity:
These factors are mainly of two types i.e. factors contributed by immunogens and factors contributed by host cells.
Factors by Immunogens:
They are size, foreignness, chemical nature, complexity, heterogenicity and susceptibility for antigen processing.
Size:
Antigens with greater than 10,000Daltons molecular weight, found to be effective immunogen and vice versa. For example: Hemoglobin is more immunogenic than penicillin.
Foreignness (Alien):
It refers to distance in phylogenetic tree i.e. evolutionary distance. Highly distance organisms found to have more immunogenicity than lesser distant one. For example: Protein from gorilla found to have less immunogenic than the protein from fish to humans because fish is more distant from gorilla.
Chemical Nature:
Depending upon the chemical nature immunogenicity varies. For example: Proteins found to have greater immunogenicity than carbohydrates, lipids and nucleicacids. Solubility also plays an important role, less soluble antigens found to have more immunogenicity.
Complexity:
As the complexity of the immunogens increases immunogenicity also increases. For example Primary structure of proteins found to have lesser immunogenicity than tertiary structure of same protein.
Heterogenicity:
In the case of multimeric proteins, heteromultimeric proteins found to have more immunogenicity then homomultimeric proteins. This was mainly because of presence of different types of epitopes in heteromultimeric proteins.
Susceptibility for Processing and Presentation:
Those antigens which are found to be easily processed by APCs, found to have greater immunogenicity than those antigens which are not easily processed. For example: Horse RBCs found to have greater immunogenicity than the asbestos.
Factors by Host:
These factors include route, genotype and dose.
Route:
Route of entry is also important to provide immunogenicity and disease. If an microorganism enters through adversal route it is degraded by immune mechanism so less immunogenic. When it enters through its natural route, it will cause disease and it also escapes from immune system partially. For example: Vibrio Cholerae when enters through circulatory system it won’t cause diarrhea; but if it enters through GI tract it cause diarrhea.
Genotype:
The genetic constitution (genotype) of an immunized animal influences the type of immune response the animal manifests, as well as the degree of the response. Natures of human beings were protected humans from some diseases and also affected by some diseases. Infection by microbes depends upon the ability to infect the human cells. It purely depends upon the genotype of microorganism.
Dose:
To induce immunogenicity an optimum amount infecting agents are antigens required and this optimum amount is known as optimum does. When microbes enters above and below this optimum dose level fluctuation occurs in immunogenicity.
|
S.No |
Parameters |
Increasing Immunogenicity |
Decreasing Immunogenicity |
|
1. |
Size |
High |
Low |
|
2. |
Composition |
Complex |
Simple |
|
3. |
Similarity of self proteins |
Multi different |
Few different |
|
4. |
Form |
Particulate and Denatured |
Soluble and Native |
|
5. |
Dose |
Intermediated |
Low and High |
|
6. |
Route |
Subcutaneous > Intra peritoneal cavity |
Intravenous and Intragastric |
|
7. |
Adjuvant |
Slow release with Bacteria |
Rapid release with bacterial component |
ANTIGENIC DETERMINANTS OR EPITOPE:
It is the region of the antigen recognized by antibodies or TCR of T cells. For example: Glucagons contain 29 amino acid residues of which N-terminal region recognized by antibodies whereas C-terminal region is recognized by TCR of T cell.
ISOLATION OF EPITOPES:
Antigens are isolated by affinity chromatography using antibody coated matrix in column. Antibodies first allowed to react with antigen of which antigenic determinant to be isolated. Unbound portion of antigens in the Ag-Ab complex was degraded by using specific proteases. After degradation, bound antigen released from antibody and antigenic determinant isolated following electrophoresis or centrifugation. By comparing the sequence of isolated fragments to original sequence of antigen, antigenic determinant region of antigen is determined.
TYPES OF EPITOPES:
There are two types of epitopes namely B cell epitope and T cell epitope.
i) B cell epitope:
It is the region of antigen recognized by antibodies. Size of this depends upon the paratope of antibodies. It is hydrophilic in nature. It is a 3D entity it may be sequential or continuous or linear peptide i.e. continuous in position (10th – 15th aminoacids). It may also be non-sequential or conformational or discontinuous peptide. Eventhough antigen contain many number of B cell epitope, only few are found to be immune dominant. B cell epitope always present on surface of the antigen. B-cell epitopes tend to be located in flexible regions of an immunogen and display site mobility.
ii) T cell epitope:
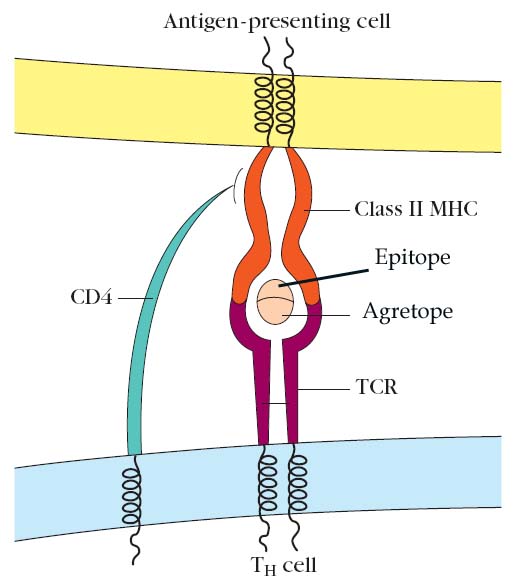
It is the region of antigen recognized by TCR of T cells. The size of T cell epitope depends upon the type of MHC present the antigen i.e. if MHC-I presents the size of epitope is 8-12 aminoacids and MHC-II is 12-25 aminoacids. It is usually present in the internal region of the antigen recognition of this epitope possible when it is presented along with MHC molecules. The position of T cell epitope which interact with MHC molecules is referred as agretope. Immunogenicity of T cell epitope achieved through ternary complex formation with MHC-Antigen – TCR of T cell.
ADJUVANTS:
Adjuvants are substances which have an ability to enhance antigenic response of antigen. Enhancing property achieved by any one or more of the following ways.
Alum is nothing but aluminum hydroxide or potassium aluminum sulphate. It acts as adjuvant by increasing the availability of antigen by the process of precipitation. Freund’s incomplete adjuvant is nothing but antigen with water in mineral oil emulsion and manidemonooleate. It is referred as incomplete adjuvant but it mainly activates humoral immunity.
Freund’s complete adjuvant is nothing but antigen in aqueous solution in mineral oil with muramic dipepetides of mycobacteria and it is referred as complete because it activates cell mediated and humoral immunity and this adjuvant have all the above four mentioned properties. Activated macrophages are more phagocytic than unactivated macrophages and express higher levels of class II MHC molecules and the membrane molecules of the B7 family. The increased expression of class II MHC increases the ability of the antigen-presenting cell to present antigen to TH cells. B7 molecules on the antigenpresenting cell bind to CD28, a cell-surface protein on TH cells, triggering co-stimulation, an enhancement of the T cell immune response. Thus, antigen presentation and the requisite co-stimulatory signal usually are increased in the presence of adjuvant. Antigen along with quil-A oil and viral proteins known as immunostimulatory complex (ISCOMs). It increase antigen ability and induce proliferation of T cells.